Hereditary Pancreatic Cancer
Aug 21, 2022
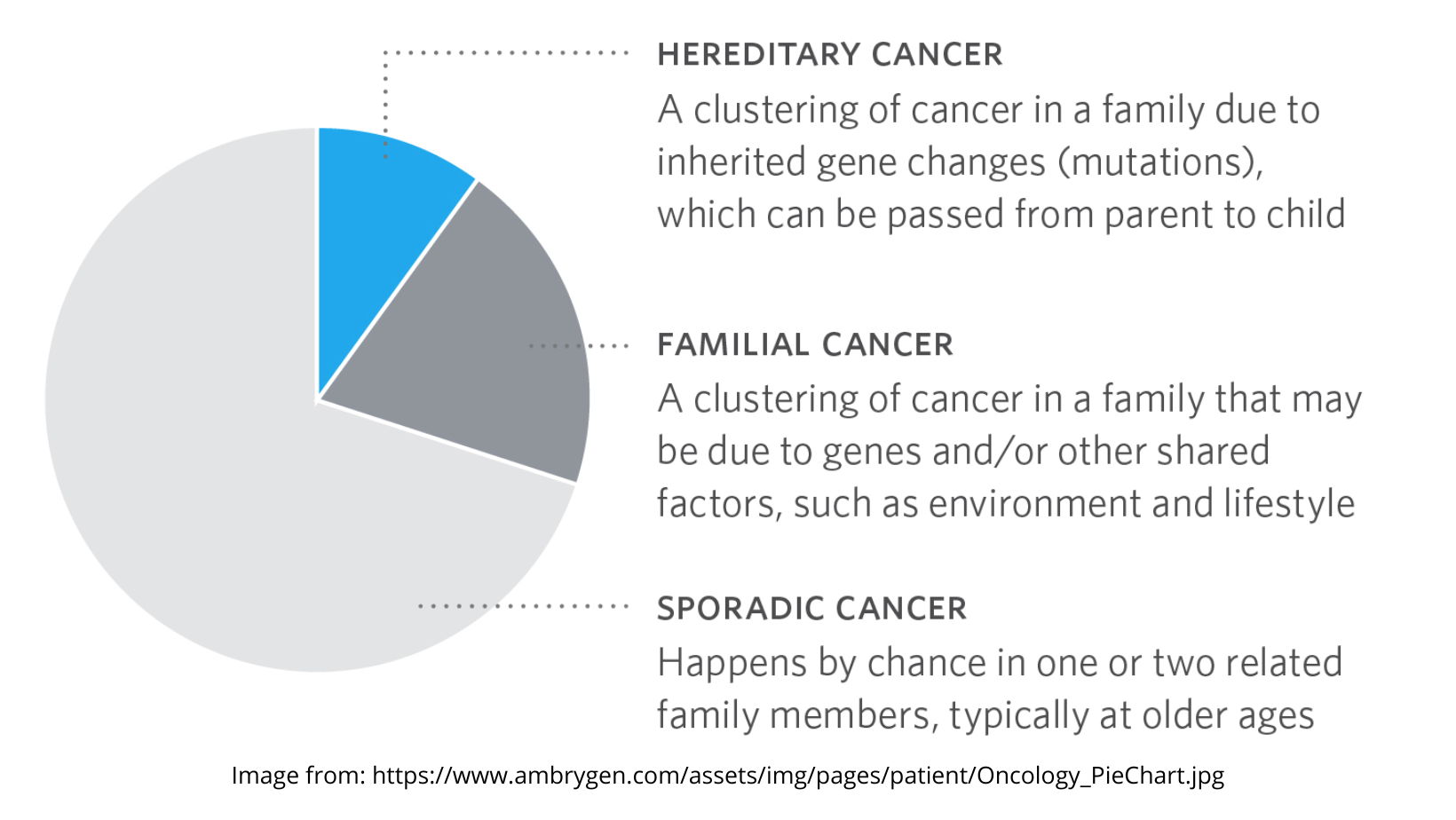
Every year, 43,000 people are newly diagnosed with pancreatic cancer. The majority of these cases are sporadic and result from random mutations or environmental causes. However, approximately 10% of pancreatic cancer cases result from hereditary genetic conditions. The low 5-year survival rate of pancreatic cancer patients increases the importance of identifying familial pancreatic cancer and monitoring those with family history of the disease.
Pancreatic Cancer and Genetics
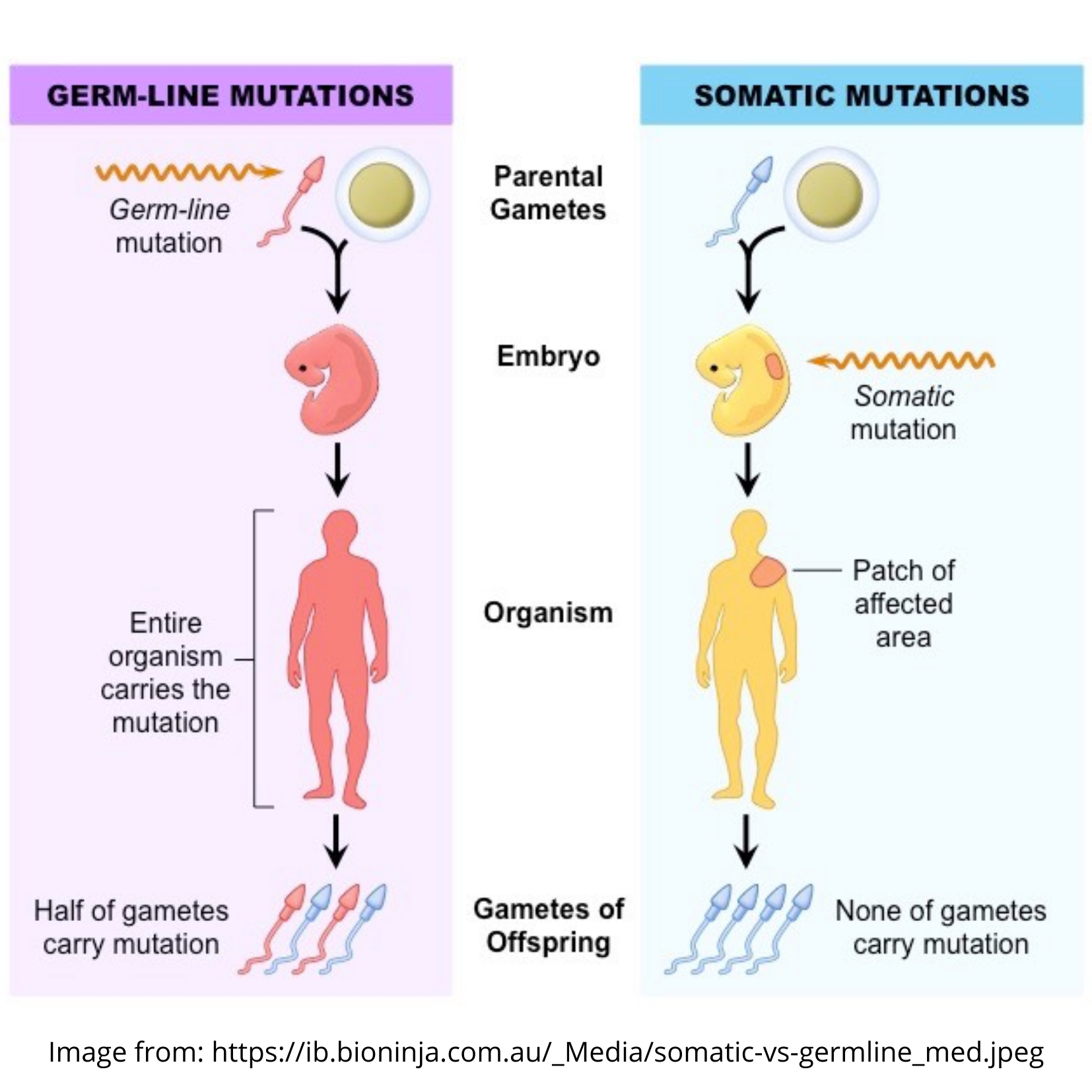
 Like all other cancers, pancreatic cancer has causes rooted in genetics. It is estimated that each cell in the human body has about 30,000 genes, which are located on chromosomes. Specific regulatory genes are involved in cancer. When these cancer-related genes mutate, or change from their initial state, cancer can result. Genetic mutations can originate from two sources: environmental causes and hereditary causes. Mutations caused by environmental factors are called acquired mutations, and mutations caused by hereditary factors are called germline mutations. Both acquired and germline mutations can cause cancer.
Like all other cancers, pancreatic cancer has causes rooted in genetics. It is estimated that each cell in the human body has about 30,000 genes, which are located on chromosomes. Specific regulatory genes are involved in cancer. When these cancer-related genes mutate, or change from their initial state, cancer can result. Genetic mutations can originate from two sources: environmental causes and hereditary causes. Mutations caused by environmental factors are called acquired mutations, and mutations caused by hereditary factors are called germline mutations. Both acquired and germline mutations can cause cancer.
Hereditary Pancreatic Cancer
The small percentage of pancreatic cancer cases that are inherited through families are caused by rare genetic diseases. There are specific familial genetic conditions that are linked to pancreatic cancer. These include:
- Defects in the BRCA1 and BRCA2 genes: Most pancreatic cancers do not result from faults in these genes. They are usually associated with breast and ovarian cancer. However, there are some cases where BRCA1 and BRCA2 mutations can be linked to pancreatic cancer, depending on family history. BRCA2 is more strongly linked to pancreatic cancer than BRCA1.
- Mutations in the PALB2 gene: PALB2 is linked to the BRCA2 gene. Mutations in PALB2 are mainly associated with higher risks for breast cancer, but they can also lead to increased pancreatic cancer risk.
- Familial Atypical Multiple Mole Melanoma Disease (FAMM): This disorder is caused by mutations in the p16/CDKN2A gene, which is typically linked to higher risk for skin and eye melanomas. However, it can also have an impact on inherited pancreatic cancer risk.
- Familial pancreatitis: Inherited pancreatitis, which causes chronic inflammation of the pancreas, can lead to pancreatic cancer as well. Familial pancreatitis is usually caused by a mutation in the PRSS1 gene.
- Lynch Syndrome: This genetic disorder is caused by defects in one of many genes. There are two types of Lynch Syndrome, and Lynch II is the one associated with pancreatic cancer. This disease results in increased risk for bowel cancer as well.
- Peutz-Jeghers Syndrome: Caused by a defect in the STK11 gene, Peutz-Jeghers Syndrome is associated with polyps in the digestive system. It also plays a role in various cancers, including pancreatic cancer.
- Ataxia Telangiectasia (ATM): ATM defects were found by Johns Hopkins researchers to be linked to pancreatic cancer. 2-3% of patients with familial pancreatic cancer have inherited defects in the ATM gene.
There is a difference between hereditary and familial pancreatic cancer. Familial pancreatic cancer is specifically defined as having at least two first-degree relatives with pancreatic cancer without a known genetic defect. Hereditary pancreatic cancer is inherited, but it does not have this particular requirement. Specific cultural groups, including African Americans and Ashkenazi Jews, have a higher prevalence of inherited pancreatic cancer as well.
Other Risk Factors
In addition to inherited genetic diseases, there are other risk factors that increase the chances of developing pancreatic cancer. They include:
- High body weight: Being overweight or obese increases risk of pancreatic cancer, along with other cancers.
- Sedentary lifestyle: A lack of physical activity has been shown by some studies to increase pancreatic cancer risk, although results have not always been conclusive.
- Age: Old age increases the risk of developing pancreatic cancer as well. Most cases occur in patients over the age of 65.
- Smoking: Heavy smoking is linked to pancreatic cancer, along with other cancers.
- Poor diet: Eating a diet high in processed foods and red meats can lead to pancreatic cancer as well.
- Pancreatic cysts: Pancreatic cysts have a risk of becoming cancerous, and those that do often form aggressive tumors.
These factors are mostly environmental and lifestyle-related, and luckily they can be avoided with lifestyle changes. Regular physical activity and a healthy, balanced diet can help minimize pancreatic cancer risk.
Managing Pancreatic Cancer Risks
Some risk factors for pancreatic cancer can be minimized, while genetic and hereditary factors are largely out of one’s control. However, certain preventive measures can be taken for patients with familial or hereditary pancreatic cancer. Knowledge is power when it comes to managing and preventing inherited pancreatic cancer, as with every other hereditary disease.
 First of all, it is important to know your family history when it comes to pancreatic cancer. Knowing which family members have had pancreatic cancer and at what age they were diagnosed is extremely helpful. If it is possible, obtaining genetic testing results from family members who have had the disease provides even more insight that can be used to monitor and prevent pancreatic cancer in future generations within the family. Seeing a genetic counselor can help determine which genetic mutations in your family are linked to pancreatic cancer.
First of all, it is important to know your family history when it comes to pancreatic cancer. Knowing which family members have had pancreatic cancer and at what age they were diagnosed is extremely helpful. If it is possible, obtaining genetic testing results from family members who have had the disease provides even more insight that can be used to monitor and prevent pancreatic cancer in future generations within the family. Seeing a genetic counselor can help determine which genetic mutations in your family are linked to pancreatic cancer.
 After finding the genetic cause of pancreatic cancer, you can enroll in a monitoring or surveillance program if you are eligible. For example, Moffitt Cancer Center has a Pancreatic Cancer Risk Management Program for those with high risk of inherited pancreatic cancer. In this program, patients receive genetic testing, a personal screening plan, and regular follow up visits. Regardless of whether or not you are eligible for such a program, making lifestyle changes such as increasing physical activity, quitting smoking, and eating a balanced diet rich in whole foods can help minimize risk of developing pancreatic cancer.
After finding the genetic cause of pancreatic cancer, you can enroll in a monitoring or surveillance program if you are eligible. For example, Moffitt Cancer Center has a Pancreatic Cancer Risk Management Program for those with high risk of inherited pancreatic cancer. In this program, patients receive genetic testing, a personal screening plan, and regular follow up visits. Regardless of whether or not you are eligible for such a program, making lifestyle changes such as increasing physical activity, quitting smoking, and eating a balanced diet rich in whole foods can help minimize risk of developing pancreatic cancer.
Summary
A relatively small, but significant portion of pancreatic cancer cases are hereditary. A wide variety of genetic disorders are also associated with a greater risk of pancreatic cancer. Some racial and cultural groups have a higher prevalence of these genetic disorders, making them more predisposed to pancreatic cancer as well.
In addition to genetic risk factors, lifestyle and environment-related risk factors also play a role in the development of pancreatic cancer. Fortunately, these factors can be controlled by leading a healthy lifestyle. Although genetics are largely out of one’s control, there are still ways to manage and prevent hereditary pancreatic cancer. With knowledge and potentially medical assistance, people with family history of pancreatic cancer can stay in control of their health and minimize risk.







